Haemorrhagic Stroke
What is Haemorrhagic Stroke?
Haemorrhagic strokes is a life-threatening emergency. It occurs when a weakened blood vessel in the brain ruptures, leading to bleeding (haemorrhage) in or around the brain.
This bleeding can increase pressure in the brain, damaging brain cells and impairing normal function, which can damage or kill brain cells.
If you think you or someone you’re with is having a stroke, immediately call 999 (or your local emergency services number). The sooner someone is diagnosed and treated, the more likely it is they’ll survive a stroke. Every second counts.

Common Causes of Haemorrhagic Stroke
Arteriovenous Malformation (AVM)
Abnormal blood vessel connections prone to rupture.
High Blood Pressure (Hypertension)
Weakens blood vessels over time.
Blood Thinning Medications (Anticoagulants)
Increase bleeding risk.
Aneurysm
A bulge in a blood vessel that can rupture.
Head Trauma
Injuries that cause brain bleeding.
Liver Disease
Affects blood clotting, increasing bleeding risk.
What is Arteriovenous Malformation (AVM)?
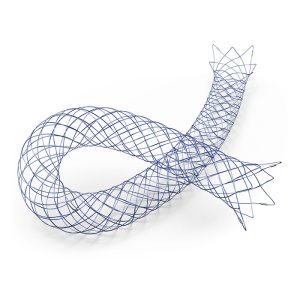
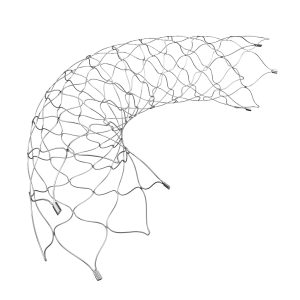
Normally, arteries carry blood containing oxygen from the heart to the brain, and veins carry blood with less oxygen away from the brain and back to the heart. When an arteriovenous malformation (AVM) occurs, a tangle of blood vessels in the brain bypasses normal brain tissue and directly diverts blood from the arteries to the veins.
When do AVMs occur?
A small number of AVMs are found at or shortly after birth. But most of them are found later, and likely form and progress later as well.
Do brain AVMs change or grow?
Sometimes, AVMs get progressively larger as the amount of blood flow increases.
What are symptoms of a brain AVM?
Symptoms may vary depending on where the AVM is located. This could include a wide variety of brain functions, such as difficulties with movement, coordination, sensation, thinking or memory, speech or vision. Severity can vary greatly.
What causes brain AVMs to bleed?
A brain AVM contains abnormal “weakened” blood vessels that direct blood away from normal brain tissue. These abnormal and weak blood vessels dilate over time. Eventually, they may burst from the high pressure of blood flow from the arteries.
How are AVMs diagnosed?
Most AVMs are detected with a computed tomography (CT) brain scan or magnetic resonance imaging (MRI) brain scan. For any type of treatment involving an AVM, an angiogram may be needed to better identify the type of AVM.
What is the best treatment for an AVM?
It depends on the type, the symptoms it may be causing and its location and size.
What are different types of treatment?
Medical therapy: If there are no symptoms or almost none, or if an AVM is in an area of the brain that can’t be easily treated, conservative management may be necessary. These patients are advised to avoid excessive exercise and stay away from *blood thinners. (*Some medications are commonly called blood thinners because they can help reduce a blood clot from forming. Common blood thinners are anticoagulants such as warfarin or heparin that slow down the clotting process and antiplatelet drugs such as aspirin and clopidogrel that prevent platelet blood cells from clumping together to build a clot.)
Surgery: If an AVM has bled and/or is in an area that can be easily accessed, then surgery may be recommended. Microsurgery allows the surgeon to work on small structures in the brain using a microscope and small, precise instruments.
Stereotactic radiosurgery: This non-surgical radiation therapy can be used to treat an AVM that’s not too large but is in an area that’s difficult to reach by regular surgery. First, a cerebral angiogram identifies the location of the AVM. Then, high-dose treatment is delivered via targeted radiation on the AVM. This method of radiation therapy causes a scar and allows the AVM to “clot off.”
Interventional neuroradiology/Endovascular embolization: It may be possible to treat part or all AVM by placing a catheter inside the blood vessels and blocking off the abnormal vessels with various materials such as glue or coils.